Keratoconus & treatment
Keratoconus

The cornea is the transparent tissue at the front of the eye, through which light travels. It is dome shaped and is responsible for the approximately two-thirds of light bending as it is focused in the eye. When the cornea becomes irregular for any reason, its power changes in a variable way, resulting visual blurring and distortion which can be functionally disabling.
Corneal ectasia is a condition where the shape of the cornea becomes unusually steep and irregular. This is most commonly seen in Keratoconus, but may also occur after laser refractive surgery (LASIK), when the cornea has been thinned to an extent where it is structurally unstable in susceptible individuals.
The exact causes of Keratoconus is currently unknown. It may be associated with:
- Vigorous rubbing of your eyes
- Other eye conditions (Including Retinitis Pigmentosa, Retinopathy of Prematurity or Vernal Keratoconjunctivitis)
- A family history of the disease in other first degree relatives
- Down’s syndrome, Sleep Apnoea, Marfan’s, Ehlers-Danlos
- History of Atopy (including asthma, eczema and hay fever)
- Patients with floppy eyelids
- Down Syndrome
- History of chronic eye rubbing
In early stages of the disease, patients will notice blurring of vision and will need increasingly frequent changes in spectacles for progressive astigmatism. In more progressive stages, good quality vision can only be obtained by wearing rigid contacts lenses and finally large scleral contact lenses. A key factor for progression of Keratoconus is persistent, habitual eye rubbing.
Rarely, a sudden painful reduction in vision heralds the onset of a hydrops event. It is caused by a rip on the delicate inner lining of the cornea and results in a deep corneal scar. Such an event usually limits the patient to full thickness graft surgery for the improvement in vision.
There are several treatment paths to follow depending on the severity and progression of the disease. The can be split into medical treatments which attempt to stabilise the disease and refractive treatments which seek to improves the functional vision.
Surgical treatments
Corneal Cross Linking
This can slow and even cause some minor regression in the progression of Keratoconus. Clinicans remain reluctant to voice that it will halt the disease but one of the longest observed groups after cross linking from Dresden after one treatment resulted in relative stability throughout the group. This procedure utilizes Riboflavin and U.V. light to strengthen the patient’s cornea by cross linking components in the stroma. Objectively it improves vision by a line or two, but most patients appreciate no dicernable change in their vision.
Corneal Transplantation
For moderate and advanced Keratoconus, where specialist contact lens fitting has failed, corneal transplantation has a place. This is a procedure where the disease cornea is removed and donor tissue is used to replace this tissue. Prior to corneal cross linking, Keratocnus patients presenting at the average age of diagnosis (23yrs) have a one in five chance of needing a corneal graft in their lifetime to aid their visual function. For patients presenting under age 17 years, their lifelong risk of needing a corneal graft is one in two! The corneal grafting rate for keratoconus as reported by the Australian corneal graft registry has dropped for the first time ever in 2015. As in other countries this has been attributed almost entirely due to the introduction of corneal cross-linking.
Refractive treatments
Spectacles
For most patients, their spectacles will have increasing levels of astigmatism correction as the condition progresses. Some of this will increasingly be irregular and thus the best correctable vision tends to drop.
Specialist Contact Lenses
For some individuals, increasingly frequent changes in spectacles may be required. Continued progression that results in poor spectacle corrected vision and this can only be corrected by wearing rigid contacts lenses. For mild to moderate disease small corneal RGP lenses work well. For more severe disease variations on scleral lenses provide comfortable good vision.
Optometrists who provide specialist contact lens fitting and follow up Keratoconus patients should be sought out to maximise non-surgical approaches to maintaining good quality vision in moderate Keratoconus.
Providing a refractive treatment without ensuring the medical disease is stabilised can last a long time. However refractive treatment alone will not last as long, will require extra re-fits and when the eye is no longer able to tolerate a contact lens is very likely to need a corneal transplant. Missing the opportunity to stabilise progressive keratoconus while prescribing rigid contact lens is becoming an increasingly indefensible position.
Corneal Crosslinking
Corneal Crosslinking with riboflavin is a treatment that increases the stiffness and rigidity of the cornea. This stabilizes the progression of corneal ectasia (such as Keratoconus). Many patients who previously had progressive ectasia have now been treated and followed for up to seven years without evidence of any further change in their condition.
Young corneas are softer than adult corneas. Younger patients diagnosed with keratoconus are higher risk of developing more advanced disease as well as an accelerated progression compared to adult onset disease. Artificial ageing of the cornea in the young keratoconus patient disproportionately and positively impacts the functional disability for these individuals.
How does Corneal Cross-Linking work?
The majority of the cornea layer is made from collagen fibers which are arranged in intersecting bundles. The strength and rigidity of the cornea is partly determined by how strongly the fibers are linked together. Over the course of a lifetime, an individual’s cornea becomes progressively stiffer due to natural cross-linking between these fibers.
Riboflavin (vitamin B2) is a naturally occurring compound which strongly absorbs UV light. By applying riboflavin to the cornea at the same time as exposing it to a UV light source, the riboflavin enhances the cross-linking effect of the UV light and absorbs the light so that the inner layers of the cornea and intra-ocular structures are protected from the any damaging effects of the light rays.
What is Standard Corneal (Epithelium-Off) Cross-Linking?
The cross-linking treatment is carried out with topical anaesthesia (eye drops). The surface epithelial cell layer is removed from the central part of the cornea, and the riboflavin drops applied. Once the riboflavin has penetrated deep in the corneal stroma, the UV light is focused onto the central area of the cornea for 15 minutes.
Afterwards, a bandage soft contact lens is applied. The contact lens is worn for three or four days until the surface epithelial cell layer has re-grown.
During the first few days the eye will be sore and watery. Sometimes there is slight haziness under the epithelial layer for the first few months after treatment, but the vision stabilizes within a month or so of the treatment.
What is Iontophoresis Corneal Crosslinking?
Trans epithelial corneal Cross-Linking (TE-CXL) is an innovative technique to treat corneal ectasia. The Trans epithelial technique is performed without removal of the corneal epithelium (the thin layer covering the cornea). Since this treatment is not invasive, it is very well tolerated, because it involves less eye discomfort and guarantees quicker vision recovery compared to the techniques that require the removal of the epithelium.
Iontophoresis (from iòntos = ion and phòresis = transport, transport of ions) consists of the transfer of molecules, with an ionic charge (among which riboflavin), throughout the tissues to be treated, by means of a low intensity electric field.
How is Iontophoresis Crosslinking treatment given?
On the day of the treatment, eye drops are used to temporarily restrict the pupil. The eye and the area around it are cleansed with an antiseptic solution. Anesthetic eye drops are used to further reduce even the slightest feeling of discomfort.
After applying a lid speculum to keep the eye open (called a blepharostat), the Ophthalmologist places an appropriate ring on the cornea of the patient, which is filled with riboflavin (RICROLIN®+).
A low intensity charge allows the riboflavin to enter the cornea. After 5 minutes of iontophoresis, the ring is removed and the treatment with low intensity ultraviolet rays is performed.
How do the different CXL techniques compare?
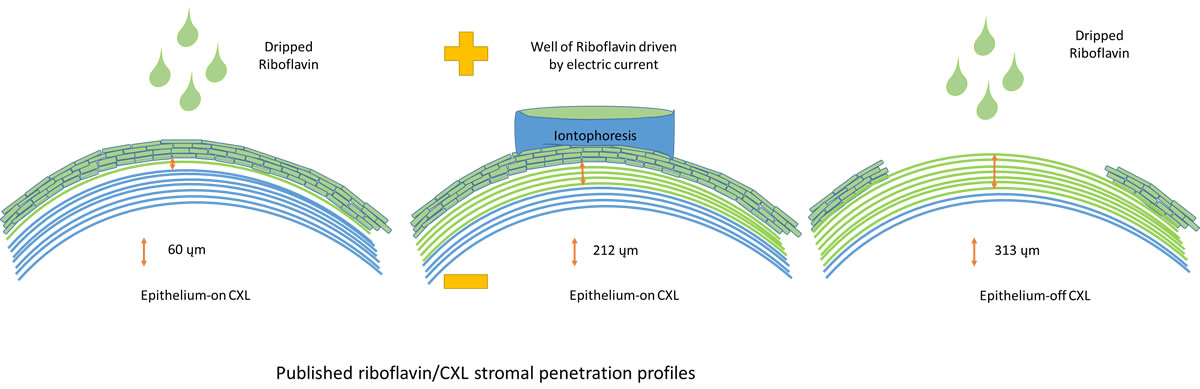
Epithelium-On CXL with dripped Riboflavin
I personally do not use this technique. It has gained prominence particularly in juveniles because of its simplicity and reduced levels of post operative pain. There is minimal penetration of the riboflavin into the corneal stroma and the riboflavin saturated epithelium acts as a barrier to CXL. There our published high 1 year treatment failure rates (60-100%). Additional preservatives are used in some products to reduce the resistance between individual skin cells and thus improve penetration. This causes large areas of the corneal skin to slough in up to 50% of patients causing pain on a par with the standard epithelium off technique. These are also the cases I would argue are more likely to note a demarcation line in the stroma and achieve the small positive flattening effects that a minority of publications have reported.
Epithelium-On CXL utilising Iontophoresis to deliver riboflavin to the stroma
The riboflavin used in CXL is in fact Riboflavin-phosphate, a charge molecule. An electric current can applied via a well on the cornea to vastly improve the delivery of the riboflavin to through the corneal epithelium (skin) to the underlying stroma. The observed CXL deep demarcation line (CXL effect limit) is 3-4 times as deep as the dripped-riboflavin epithelium-on technique and about 2/3rds the depth obtained with the standard epithelium off technique. It is less painful and recovery takes 1-2 days compared to the standard epithelium off technique which requires 1-2 weeks. The risks of infection are virtually zero as there is usually no skin defect. The risks of infection, haze, scar and 2 lines decreased vision are much lower (not reported….yet!) while because there is less cross linking the risks of continued progression are theoretically somewhat higher.
I reserve this for patients with mild to moderate keratoconus who have good unaided vision in whom the risks associated with standard epithelium off CXL, particularly if they have only one good seeing eye are considered too high. Although the theoretical risks of continued progression are higher with this form of CXL treatment, when using for milder disease there is also a trade off as these Iontophoretic CXL cases are less likely to progress as much as moderate-to-severe disease would. Published literature shows continued progression rates similar to that associated with standard epithelium-off CXL. What is different is that it does not cause regression of keratoconus as it can with the standard epithelium-off technique which is no big loss as they only have this procedure when they are seeing well anyhow.
Epithelium off standard CXL
The skin is removed and the riboflavin dripped on. The post op recovery to baseline vision is usually 1-2 weeks and if you drive to work the glare could impact you for longer. It provides maximal cross linking. 60% experience a flattening response by 1-2 years post op. The risks for moderate progressive keratoconus include a 5% risk of each of the following; scarring, 2 lines decreased vision and continued progression.
The risks for excess scarring include a very steep cornea, a very thin cornea and age over 35. There is a generally respected 400um safety margin where the cornea should be thick enough before starting CXL. In severe cones to avoid or as a prelude to corneal transplantation these corneas are swelled using hypotonic riboflavin after removal of the corneal epithelium, generally it adds about 120um thickness and thus provides the generally accepted barrier to irradiation of the corneal endothelium. It is however reserved for patients who are older, with more severe disease and thus by default the risks of scarring after CXL are also greater in this group.
What variations on the delivery of CXL exist
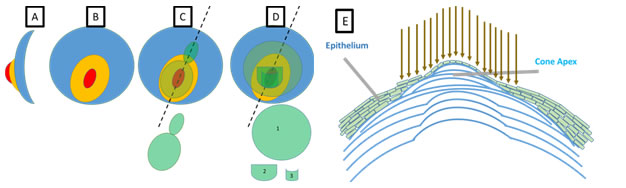
Figure: (A) The side view of the conical shape of keratoconus. (B) the en-fasse or topographic view of keratoconus (C)+ (D) represent two examples of the segmental application of CXL. (C) Topographic guided CXL applies more treatment to the cone and less or no treatment elsewhere on the cornea (D) Alternative topographic techniques apply a large circular standard treatment area (1) and then apply supplemental treatment zones to the most diseased part of the cornea (2) and finally the cone apex (3). In both these cases significant and deliberate over treatment of the most thinned, disease part of the cornea compared to the original standard Dresden protocol (5.4mW/cm2) occurs. The scar rate and deep persistent haze theoretically should be higher but this information is to date not forthcoming in my reading of the literature and therefore I do not advocate its use but look forward to seeing more publications from others on the subject. (E) Uses excimer laser to reshape the cornea immediately prior to standard CXL. The skin (epithelium) is thinner over the apex of a cone. The technique known as trans-epithelial phototherapeutic keratectomy (PTK) uses the skin as a mask so that laser ablation of the diseased stroma preferentially occurs over the cone apex as the laser ablates through to the underlying corneal stroma first. This improves the shape of the cornea, which then undergoes standard CXL. When the epithelium heals it does so with a more uniform thickness. This technique is particularly useful if there is some inherent axial myopia (about one in 10 keratoconus patients), especially in those with highly asymmetric disease.
Variations on Keratoconus
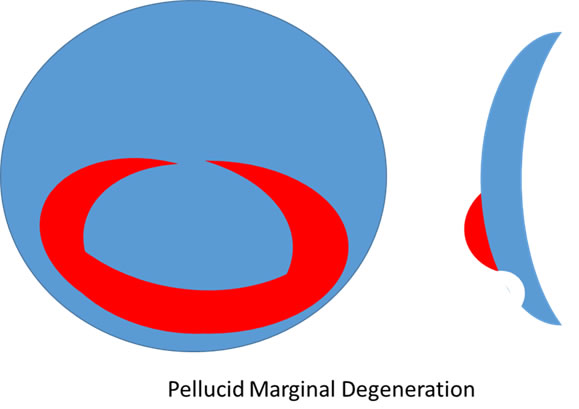
Pellucid marginal degeneration can be viewed as a peripheral form of keratoconus. The thinning starts 1mm in from the limbus and can extend in a broad are for about 150 degrees. Corneal topography produces a classic crab claw pattern on extended 12mm measurement maps. It can occur at any age and progress at any rate but generally presents much later (4th-5th decade) and significant further progression takes a decade to occur. It is much less common than the more central occuring Keratoconus and spectacle corrected astigmatism is possible until quite late. There is much less published literature on CXL in PMD as it is rarer and takes longer to define stability but modest positive evidence on both the safety of CXL in PMD and its ability to stabilise the medical condition have been published. Extra care is required not to irradiate the limbus in these patients as there is a theoetical risk of producing Ocular surface squamous neoplasia (OSSN), dysplasia of the limbal self renewing (stem) cells.
Complications of CXL
For moderate progressive Keratoconus the best pulished literature suggests there is a 5% risk of ech of the following
1. Scar
2. 2 lines of reduced vision (either unaided or best corrected)
3. Continued progression
These risks can be further stratified so that excess risk occurs if
1. Age over 38
2. Great corneal steepness (Kmax (on Pentacam) greater than 58 D)
3. Thinnest corneal pachymetry (Less than 400um)
Retinal Surgery
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Am I suitable?
Use our online tool to find out if you’re suitable for Laser Eye Surgery or cataract surgery.
