Eye Conditions
Please view the list of Eye Conditions on the left. We discussed a few conditions here for your information and to help you on your journey of healing.
Some eye conditions can affect your vision and correction of the condition will depend on your individual circumstances. Some eye conditions can get worse with age and the sooner it is treated, the better for your quality of life & the easier it is to treat them. Should you have any concerns about the health of your eyes, we would advise you to visit your nearest Eyes Matter clinic
Acute Angle Closure Glaucoma
Emergency Eye Condition
Acute Angle-Closure Glaucoma is where there is a sudden rise in pressure; it can occur within a matter of hours. It is an ocular emergency as the eyesight can be permanently damaged if treatment is delayed.
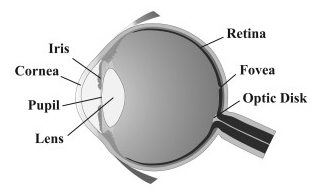
It occurs when the colored portion of your eye (iris) is pushed or pulled forward. This causes a blockage of the drainage angle of the eye.
The flow of clear fluid in the eye starts behind the iris comes through the pupil and leaves via a circular drainage channel at the base of the front surface of the iris. When it is blocked, the eye’s internal pressure (intra-ocular pressure) will spike and damage the optic nerve at the back of the eye that transmits images from the eye to the brain.
Acute Glaucoma attacks are not always a full onset case. Patients can suffer a series of minor attacks. Symptoms of Acute Angle Closure attacks include:
- Blurring of vision
- Halos (rainbow colour rings around lights)
- Severe Pain
- Redness of the eye
- Nausea and/or vomiting
An attack of Acute Angle Closure Glaucoma can be stopped with a combination of drops; and tablets or injections. Treatment is directed towards breaking the attack by reducing the intra-ocular pressure which help clear the from window of the eye ‘the cornea’. As soon as the cornea clears to a safe level, the eye specialist will perform a laser iridotomy (a small opening in the peripheral iris). This will allow the fluid to flow more freely through an alternate drainage channel and so the eye pressure drops. The laser procedure is relatively painless and patients usually gain very rapid pain relief.
The entire procedure should take less than five minutes but a lack of corneal clarity sometimes means the procedure has to be delayed. Laser surgery may be performed prophylactically on the other eye as a preventive measure. This is typically done before you leave hospital or clinic, such is the perceived risk usually to the other eye.
Acute Corneal Graft Rejection
If you have a corneal transplant along with the following symptoms:
- Diffuse redness and congestion appearing around the white of the eye;
- Increasing light sensitivity;
- A sudden reduction or blurring of vision;
- New onset of an ocular ache OR pain in the eye, you may be having an Acute Corneal Graft Rejection.
It is imperative that you seek medical advice as soon as reasonably possible.
Situations that might provoke a graft rejection episode include
- The first 2-8 weeks after finally stopping the steroid drops.
- During an acute viral or flu-like illness or after vaccination.
- It is generally advisable to restart or increase your topical steroid temporarily during this period of stress.
However, medical direction and supervision should always be sought first where possible. If you are in a remote area start drops every hour by day and seek review with an eye specialist within 48 hours if possible.
CLINIC TELEPHONE NUMBER : 3193-1100
CLINIC FAX NUMBER: 3193-1101
Anterior Segment Reconstruction
Anterior Segment Trauma of the eye is a commonly seen medical injury. It typically presents to eye casualty as an acute scenario.
It can involve either penetrating or blunt injuries to the eye. If left untreated, these injuries can lead to devastating consequences, such as loss of vision or loss and severe infection. The most important rule is to put the eye back together with minimal delay, and to reform the anatomy of the eye as close to normal as is possible.
Anterior Segment Reconstruction
Anterior segment injuries include injuries to the eyelids, conjunctiva, cornea, iris, and the lens of the eye. Treatment options vary wildly due to the various factors that play a role in any injury. Mild trauma cases such as a small ocular surface foreign body may only require in-office treatment. Whereas extreme cases such as penetrating wounds require emergency surgical closure.
More serious and complex cases may require multiple surgical interventions.
When globe integrity and stability has been achieved in chronic cases, treatment options can follow on from globe preservation towards cosmetic and functional visual rehabilitation.
It is important that any further intervention is weighed against the risks of further destabilisation of these previously injured eyes, in particular the justification of operating on that eye has limited visual potential.
Numerous causes exist. If you are concerned about your genetic or environmental factors, contact us for a consultation
Anterior Segment Trauma can bring pain and vision loss.
Corneal Reconstruction
In cases of corneal reconstruction after trauma, every effort should be made to conserve a patient’s own cornea when there is the prospect of preserving reasonable functional vision.
The insertion of hard contact lens and performing a check for spectacle requirement over the top, can act as a diagnostic tool of residual functional vision, and provide a measure of potential functional rehabilitation for the affected eye. If hard contact lenses are not tolerated, the use of laser and implant corrections as an alternative to treat any optical disturbance can restore useful vision. If the patient’s own cornea offers no prospect of functional vision, treatment with corneal transplantation may be appropriate.
Iris Reconstruction
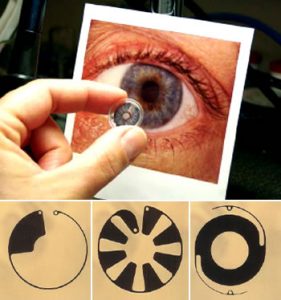
Reconstruction with an artificial iris can take many forms. The traumatised iris can be re-sutured to provide an acceptable contour and colour to improve cosmesis.
Artificial iris inserts can be individually painted in an attempt to match the other eye. Other implants are black and simply seek to improve functional vision by reducing glare caused by the aberrant light.
Depending on the trauma to the iris, various styles and shapes for the artificial iris are available to treat most cases.
Iris Base Trauma
The base of the iris is prone to damage during ocular trauma. This can lead to abnormal intra-ocular pressures (either high or low). Both can cause visual loss, and require immediate or delayed intervention to limit damage to the visual potential of the eye.
In most cases, the pressure in the eye is normal but may slowly rise years after the initial trauma. Appropriate follow up for severe injuries needs to be undertaken in those at risk.
Traumatic Cataract
A Cataract is an opacification of the natural lens of the eye. When it impairs the visual pathway, removal is required to improve vision. In cases of traumatic cataract, there is the added concern that the lens capsule could be breached. Leaking lens material into other parts of the eye can cause dangerous intra-ocular pressure rises. Not only that, the lens material itself can induce severe inflammation in the eye. The combination of severe inflammation and high pressure rises can cause irreversible damage long after the initial insult.
Fluid can also leak into the lens through a small capsular rupture. Occult capsule rapture can cause distention and further opacification in an eye that initially looked to have minimal lens damage. This can lead to extension of the lens capsule tear in the eye, and initiate delayed severe inflammation and pressure rise.
Consequently, severe trauma to the eye needs to be monitored closely in the early stages to pick up such events. In rare cases, an isolated peripheral lens breach can be glued using tissue glue which limits cataract formation, and avoids the need for cataract surgery.
Posterior Segment Trauma
Any severe damage to the front of the eye can damage the back of the eye, and therefore the visual potential of the eye. This may be obvious (retinal detachment), but it may also be occult, and vigilance in the initial examination as well as during follow up is required to limit the long term impact of any such injury. Special ultrasound scans help us assess the back of the eye even when no direct view is possible initially.
Blepharitis
Blepharitis is a condition where the rims of the eyelids become inflamed. This can cause your eyes and eyelids to become red, irritated and itchy.
Blepharitis is a chronic condition. It is estimated that it is responsible for 5% of all eye problems that are reported to general practitioners. The condition is more common in older adults, though it can develop at any age.
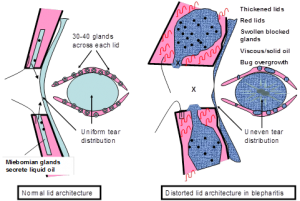 The exact cause of Blepharitis is unknown. One of the main reasons postulated is that the oils, which are normally liquid at body temperature, are turned to a sludge or solid state by an overgrowth of normal bacterial flora which metabolize the oil thickening it up. This then blocks the glands, leading to inadequate amounts and poor quality oil in the tear film.
The exact cause of Blepharitis is unknown. One of the main reasons postulated is that the oils, which are normally liquid at body temperature, are turned to a sludge or solid state by an overgrowth of normal bacterial flora which metabolize the oil thickening it up. This then blocks the glands, leading to inadequate amounts and poor quality oil in the tear film.
These factors induce inflammation on the ocular surface to variable degrees, but not usually causing overt infection. Finally, a viscous circle ensues of increasingly viscous oils in the glands leads to blockage of the glands, chronic dilatation of the glands and loss of normal architecture and function.
Most people will experience repeated episodes of blepharitis and then have long periods of time where they do not have any symptoms. Symptoms tend to be worse in the morning, and both eyes are typically affected.
Symptoms include:
- Itchy, sore red eyelids
- Eyelids stick together, difficulty opening the eyelids on waking due to matting
- Eyelash encrustment
- Burning, gritty sensation in the eyes,
- Increased sensitivity to light (photophobia),
- Abnormal eyelash growth
- Loss of eyelashes
Pre-existing skin conditions such as Rosacea or Seborrhoeic dermatitis
 Developing a regular routine of eyelid hygiene is essential in the long term treatment of Blepharitis. It is important that you clean your eyelids every day, whether or not you are experiencing any symptoms. You should consider it part of your daily routine, like showering or brushing your teeth. Effective eyelid hygiene will reduce both the severity and frequency of symptoms.
Developing a regular routine of eyelid hygiene is essential in the long term treatment of Blepharitis. It is important that you clean your eyelids every day, whether or not you are experiencing any symptoms. You should consider it part of your daily routine, like showering or brushing your teeth. Effective eyelid hygiene will reduce both the severity and frequency of symptoms.
A trilogy of fist hot compresses to the lids, then lid massage and finally a mild detergent lather to the lid margins form the core of this very mundane but effective management. Blepharitis cannot be cured only kept in check with regular lid hygiene if problematic.
In more severe cases, the use of antibiotic ointments or tablets may be recommended if there is no improvement in symptoms after a longer period of regular eye lid hygiene.
Bullous Keratopathy and Fuch’s Corneal endothelial dystrophy
The cornea is a transparent tissue at the front of the eye through which light travels. It is dome shaped, and is responsible for most of the focusing of light onto the retina. When the cornea becomes waterlogged for any reason, it is less transparent and the vision is reduced.
Fuch’s corneal endothelial dystrophy
4% of the population have this condition. It usually runs in families and is usually not important. It impacts the health of a single layer of cells on the internal lining of the cornea that are responsible for pumping fluid out of the cornea. They do not divide and those that you are born with are the ones you die with. It is this layer that is damaged when bullous keratopathy exists. The cell density of this layer reduces with age.
In Fuch’s the cells decay at a faster rate and after cataract surgery the curve is reset at a much lower level. It becomes important when Fuch’s patients undergo cataract surgery. It is important that it is identified before surgery and specific additional steps taken to minimise the impact on this single cell layer during cataract surgery. Sometimes it will be inevitable that the cornea will stop working after cataract surgery and here a combining cataract surgery and Corneal Transplantation may be the faster most reliable way to ensure visual rehabilitation.
Symptoms vary. In early disease patients may notice a fluctuation in their vision throughout the day, worse in the mornings. As the disease progresses, it takes longer for the vision to clear in the day. Finally, the cornea is permanently waterlogged, the vision reduced and the skin of the front of the eye is easily scratched leading to pain, light sensitivity and watering eyes.
So patients do not feel their vision is impacted even though tests confirm the vision is affected and they have marked water blisters and water logging of the front of their eyes on microscope examination. This is because the problem creeps up on them slowly. Once the waterlogging causes blistering (bullous keratopathy) then secondary scarring can limit the usefulness and final vision obtainable with the newer standard partial thickness transplant techniques.
How can these symptoms be controlled?
In the earlier stages of the disease hypertonic salt drops (Muro128) and even use of a hairdryer can improve the vision earlier in the morning. These treatments have no effect in moderate to late disease. Corneal grafting can offer some patients improvement in vision and comfort. In some although the drops improve the vision they may cause unacceptable irritation and redness causing the eye to become more inflamed and create a more hostile environment for any final corneal transplant.
What is a corneal graft?
A corneal graft for Fuch’s or bullous keratopathy is perceived as a tissue rather than an organ transplant. Tissue gifted from a donor and finally the grieving family of the donor. It is used to replace the defective cornea in the patient. A corneal graft for bullous keratopathy can be a full thickness graft (man-hole cover) or a partial thickness graft (wallpaper). A full thickness graft requires sutures for up to 2 years to keep the graft in place, and although compatible with the highest level of vision possible, is more often associated with large amounts of astigmatism which mean only about half of recipients will be correctable to 20/20 after the operation. Up to half of patients require contact lenses to get the best vision, or tolerate a lesser level of vision in spectacles. Furthermore, after sutures are removed the shape of the graft can change significantly. Incisions in the graft, laser to the graft surface and implants into the eye can all be helpful in maximising the final best corrected vision. The vision may require 3 yrs and 12-14 outpatient visits to stabilise and maximise the vision.
A partial thickness (posterior lamellar graft) requires no sutures in the graft itself and is stuck to the back of the patients own cornea using an air bubble and is able to remove the water-logging from the patients own cornea. The vision is not quite as good as with a full thickness graft but the majority of patients can expect to maintain driving vision if there is no other problem with the eye. The vision recovers much more rapidly (12 weeks) with about 60-80% of otherwise normal eyes having a best corrected vision within driving standards by 6 months. Additionally as the patients own cornea remains intact and there are no large wounds or sutures there is usually much less astigmatism distorting the vision. Typically 4-6 outpatient visits over 2 years are required.
Partial thickness grafting is rapidly becoming the new gold standard for patients with bullous keratopathy requiring a corneal graft. Common terms for this procedure depend on the exact technique performed; Descemet’s stripping endothelial keratoplasty ( DSEK / DSAEK ) or Descemet’s membrane endothelial keratoplasty ( DMEK ). It is however not the right operation for everybody. The surgeon will discuss with you what is the best option based on your individual needs.
What does the surgery involve?
With any corneal graft it is useful to think of this as a process and a journey rather than a one off surgical event. The surgery can be carried out under general anaesthesia or local anaesthesia with sedation. With a full thickness graft sutures are required. These may need to be adjusted within the first couple of months to reduce astigmatism and maximise the intermediate post-operative vision. Sutures are then removed around 18-24 months. A posterior lamellar graft (partial thickness) is held in position on the back of the patients own cornea initially by an air bubble for 20 minutes at the end of surgery while lying on your back. This air bubble needs to be repeated in up to 2-5% of cases to ensure the donor transplant remains attached.
What results may I expect?
The outcomes of corneal transplantation have been most extensively studied using data from the Australian Corneal Graft Registry. Broadly, these outcomes can be divided into two major groups: Visual outcomes and survival outcomes. Both groups depend very much on the condition of the eye prior to the graft being performed. Conditions which have resulted in inflammation, infection or blood vessels entering the eye e.g. herpes simplex infections are associated with worse outcomes than those which do not e.g. keratoconus. A prior blood transfusion and a failed previous graft are also recognised as risk factors (albeit lesser) for graft survival. Overall, approximately 60% of grafts are functional at 10 years (rising to >90% in the best cases).
Visual outcomes vary according to the reason for which the graft was performed. A patient with uncomplicated Fuchs’ dystrophy might expect to achieve 6/12 vision at 5 years about 50% of the time with a full thickness ( penetrating ) graft. These figures are a guide and assume no other ocular disease. It has been estimated that approximately 40% of patients would achieve their best possible vision following a full thickness corneal transplant by the use of a contact lens but a quarter-of those individuals cannot use one because of difficulties in the handling of the lens.
A study which looked at patient satisfaction following corneal transplantation found that overall, about 75% of patients were satisfied. Partial thickness corneal grafts are less likely to need contact lenses to maximize their vision however their visual potential is usually 1-2 lines less than with a full thickness graft but up to 15% can still expect to achieve 20/20 corrected vision in the longer term but between 60-80% can be corrected to within driving limits.
Are there any risks with the surgery?
All operations carry the risk of complications whether from the anaesthetic, surgical procedure, subsequent medical procedures (e.g. removal of stitches) or any drugs e.g. eye drops which need to be taken. Specifically, in the case of eye surgery in which a cut is made into the eye, there is a risk of infection or bleeding inside the eye which can cause a permanent worsening or (rarely) loss of vision. The risk of retinal detachment following a corneal transplant is estimated at about 2% (twice that for cataract surgery), and sight threatening infection about 1% (five times higher than for cataract surgery). The donor material is tested for HIV, Hepatitis and the presence of bacterial infection and is assessed for quality at the supplying Eye Bank.
There is always however, remains a risk that a transmissible disease may be passed from the donor to recipient although that risk is thought to be extremely small.
All transplant operations rely on the body’s own tendency to reject foreign tissue to be medically suppressed. There is always a risk of graft rejection. This runs at 15-30% for full thickness grafts.
Partial thickness grafts are more likely to dislodge inside the eye (1 in 10) within the first week of surgery and can usually be replaced with another air bubble easily. The extra tissue handling involved in a partial thickness graft and the need for repeat air bubbles means that the risk of early graft failure is slightly higher than with full thickness grafts. It is hard to be sure but about 1-5% (versus 1% with full thickness grafts).
The long term data for posterior lamellar grafts has not been published yet as this is a new operation however it seems that rejection rates of less then 1-3% can be expected. However unlike a full thickness graft a failed partial thickness graft is simply peeled off and another new graft inserted relatively easily. A DMEK is very thin and fragile. This type of transplant gives the best possible visual outcomes but also the highest rate of primary graft failure with some estimates for primary graft failure being as high as 1 in 3. This raises ethical issues regarding the commodification of donor material as well as the additional demands on a precious resource.
Cataract
A cataract is a clouding of the eye’s natural lens. The lens is normally completely clear.

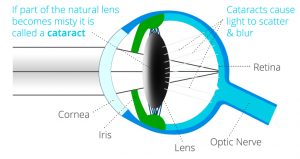
Normal Clear Lens (left) / Cataractous Lens (right)
However, when a cataract forms, the lens slowly becomes discolored (yellow or white). Because the lens focuses light inside the eye, vision slowly becomes blurry as a cataract forms.
Cataract is the leading cause of blindness throughout the world. While easily treated with surgery, most people affected by cataracts are not aware it can be successfully treated.
Cataracts occur predominantly in people aged 60 or over, as part of the normal ageing process. It can also occur in people as young as 40 due to other risk factors. The development of cataracts is similar to other age-related changes in the human body.
Risk Factors:
Risk factors for development of Cataracts include:
- Older
- Diabetes
- Smoking and alcohol use
- Prolonged exposure to sunlight (U.V light)
- Trauma and previous intraocular surgery
- Long term use of steroid based compounds
Patients with Cataracts can expect common symptoms that include:
- Cloudy or blurry vision.
- Fading of colours
- Glare from light sources (such as headlights, lamps)
- Sunlight may also appear too bright
- Halos may appear around light sources.
- Poor night vision (especially when driving).
- Double vision or multiple images in one eye. (This symptom may clear as the cataract gets larger.)
- Frequent prescription changes in your eyeglasses or contact lenses.
Depending on the visual impairment and progression of the patient’s Cataracts, there are a few choices to improve visual acuity.
Prescription Glasses
Patients with cataracts can update their spectacles at the first instance to avoid surgical intervention. Once the cataract progresses, it will impede the distance visual acuity and the law of diminishing return applies with respect to the benefit of further spectacle updates.
This procedure is the removal of the cloudy lens along with the insertion of an artificial intra-ocular lens to take its place. There are several different types of procedures to remove the cataract. The most commonly utilized technique is Phacoemulsification with Insertion of an Intra-Ocular Lens.
Phacoemulsification and Intra-ocular Lens implant
The purpose of surgery is to replace the cloudy lens with a clear lens implant inside the eye. Phacoemulsification is the procedure where the cloud lens is removed through a small incision (@2mm) in the cornea. The thin clear membrane (capsule) holding the cataract is left intact to support the new lens implant. A thin ultrasound probe is inserted into the eye that uses ultrasonic vibrations to dissolve the lens. These tiny fragmented pieces are then suctioned out using the same probe. Once the cataract is removed, an artificial lens is placed into the same thin capsular bag that the cataract occupied. This intraocular lens is essential to help your eye focus after surgery.
It is unusual to require a stitch in the eye at the end of the operation because the incision is so small it is nearly always self-sealing. Eyes that have a thin corneal wall (keratoconus) tend to be floppy and these do require a stitch to avoid wound sag and degradation of the expected visual outcome.
This procedure requires the use of anaesthetic. Topical anaesthetic drops, such as eye drops and sedation work well. Although eye drop anaesthesia does not numb the eye completely it does provide very effective numbness. Occasional pressure on the eye is all that is likely to be felt at certain points during the operation but sharp pain is very uncommonly reported by most patients. Larger volumes of anaesthetic can be deposited around the eye and can stop the eye moving as well as feeling anything at all (peribulbar or subtenons)
Lens Selection: What sort of vision do you want after the operation?
Depending on an individual’s needs, there are several different intra-ocular lens options available to suit a various ranges of demands. The information below is a brief insight to options available to a patient. Consultation with a specialist Cataract & Refractive surgeon is always required to ensure the patient is suitable for a specific lens type.
Single distance vision (SDV) lens Implants
This utilises a lens with a single focal point, usually set for distance in each eye. It gives good binocular vision over a useful range. If a patient is happy to wear intermediate and reading glasses, then this is the most common option and is usually the only option offered in the public health system.
Monovision
Two different standard lenses (one eye set for distance vision, the other set for intermediate distance vision), then this is a suitable option for those patients who may have had prior experience of it in spectacles or contact lenses. It breaks down stereopsis (3D perception) and you will still need reading glasses for fine print. If you have not tried it before then doing so for the first time at cataract surgery is not the wisest choice. In my practice I reserve this for those who have had experience of this naturally or in contact lenses, for most others tolerance is untested and cataract surgery is not the best place to first try it.
Micro-monovision
One eye is set for distance the other for an intermediate focus point. This is well tolerated as still provides some stereopsis (3D perception) useful range of vision but you will still need readers for all near tasks and occasionally for visual tasks performed at an intermediate distance. This is another very common choice and if the patient is happy to wear readers, you have very happy patient indeed.
Accommodating lens implants
These are lenses that move when implanted in the eye and try to mimic the body’s own natural lens movements. They aim to give good vision over a range of distances. In reality because they move their resting point in the eye is more unpredictable and more people end up a little more short or long sighted than they bargained for. Also most do not move enough and so you still need reading glasses for near and move too slowly so there is a significant lag time ( speed of accommodation ) when you look from the distance to focus on something up close which can be quite frustrating. Others accommodating lenses move too easily in a bid to obtain more near vision and there are a few anecdotes that with a good sneeze one can apparently be left short sighted unexpectedly.
Multifocal Lens Implants
This lens type has both a distance component and reading component. This work in a similar manner to bi-focal prescription glasses except that in glasses the patient looks from the distance into the near add and thus the whole vision sees only one in focus image. With multifocal lens implants both the distance and the near vision are in focus at the same time. When one looks in the distance there is usually nothing obstructing the view at near. When looking at book for near vision, the book blocks the distance image. Multifocal implants offer patients relative spectacle independence and the same operation is offered as a life style choice to patients without cataract who simply want the greater freedom from wearing glasses. They are often referred to as a premium lenses ( a marketing term ) but they truly are more expensive. A period of adaption is required and the compromise with this lens is often noted at night with ghosting, halos and excess stray scattered light. This is most notable when viewing a point source of light at night (e.g. a car headlight).
Not all multifocal implants are the same. Some of the cheaper versions are based on simple prism technology with concentric rings of distance and near which have been around for 25 years and the technology has not changed significantly in that time in my opinion. These diffractive multifocals produce marked halos and light scatter particularly troublesome when night driving. So much so I refuse to offer this particular type of implant as the adaption phase is typically 6-12 months and a significant percentage of individuals remain dissatisfied and less confident with night driving. It also can have a significant explant rate when advocated to the wrong type of patient.
Personally I prefer the segmental multifocal implants. The adaption phase is 4-8 weeks typically and the impact on night driving confidence is consistently reported as much less. Here the near vision is inferior to the distance segment. The aberrations in the vision happens in the vertical meridian (inferiorly) as opposed to the diffractive multifocal implants that produce the 360 degree multiple ring halo effects.


Extended depth of focus and Extended range of vision implants
Here the discussion on optics ranges to the blending of technologies between diffractive IOLS with their course transition and the segmental IOLs with their slow transition from distance to near. Others describe the effect an oil droplet on the lens. A dog with a different tail is my preference. While EDV is the new black on the marketing scene. Reasonably well tolerated….apart that is with the 7% with significant Halos in the FDA trials make this lens like vegemite. You love or you hate it. A potential explant rate approaching in in ten in not my idea of sleeping well. My perception of its relative unpredictability means it has no place in my practice.
Toric lens implants
Patients with high levels of astigmatism can utilise Toric Lens technology, which is designed to counter-act this refractive disorder. Toric lenses correct distortions in one particular meridian/ axis. They can be found in single distance vision lenses and in multifocal implants. Correcting astigmatism is the second most important optical correction, impacting the quality of the unaided visual outcome after correcting defocus, (how long or short sighted a patient is).
Diabetic Eye Diseases
Diabetic Retinopathy is the most common diabetic eye disease, and a leading cause of blindness in Australia. It is a complication of diabetes that damages the blood vessels in the eye. All people with diabetes are at risk of this eye condition.
Over time, too much sugar in your blood can lead to the blockage of the tiny blood vessels that nourish the retina, cutting off its blood supply. As a result, the eye either accumulates fluid (oedema) or attempts to grow new blood vessels. In particular these new blood vessels don’t develop properly are fragile and can leak easily.
There are two types of diabetic retinopathy.
In the early stages of diabetic retinopathy, you may not experience any symptoms. As the condition progresses, diabetic retinopathy symptoms may arise and these include:
- Spots or dark strings floating in your vision (floaters)
- Blurred vision
- Fluctuating vision
- Impaired colour vision
- Dark or empty areas in your vision
- Vision loss
It is important to note that Diabetic Retinopathy usually affects both eyes and regular screening of known diabetics is important to pick up early disease before the vision is affected and effect early treatment to limit the potential for vision loss in the years ahead.
Any patient with diabetes can develop diabetic retinopathy. Risk factors associated with this condition include:
- Duration of diabetes
- Poor control of your blood sugar level
- High blood pressure
- High cholesterol
- Poor lipid control
- Pregnancy
- Smoking and/or tobacco use
Dry Eyes
Dry Eyes (also known as Keratoconjunctivitis sicca) is caused when the eye gland doesn’t create enough tears to stay wet. It can make your eyes feel uncomfortable or sometimes cause problems with vision.
Dry eye is common and can be treated with eye drops or small changes to your lifestyle.
Eye Infections
Types of eye infections
Conjunctivitis (Pink eye)
Conjunctivitis is an eye infection of the sclera (white of the eye) and it can be caused by bacteria, viruses, chemicals, foreign body or allergies.
Symptoms of conjunctivitis include:
- Eye irritation and redness
- Excessive tearing of the eyes
- A discharge of pus
- Swelling of the eyelids
- Light sensitivity
Patients must follow good personal hygiene such as washing their hands with soap, avoid sharing towels or cloths; along with, avoiding contact with others while discharge is still present. The treating doctor may prescribe antibiotics. Patients should see their doctor as soon as possible to ensure there is no permanent damage from this condition.
Keratitis
Keratitis is inflammation or irritation of the cornea (the clear, domed shape tissue in front of the eye). It can be caused by infections such as; bacteria, viruses, fungi and parasites or it can have non-infectious causes; such as minor injury, dry eyes or other diseases.
Symptoms of Keratitis include:
- Eye pain
- Eye redness
- Excess tears or discharge
- Difficulty opening the eyelids
- Blurred vision
- Decreased vision
- Light sensitivity
- Foreign body sensation
Keratitis can be classified by its location, severity and cause. It can be acute or chronic and examination on the slit lamp is important. Pathology samples may be sent off depending on the clinical presentation. Patients should see their doctor as soon as possible to ensure there is no permanent damage from this condition.
Uveitis
Uveitis is inflammation of the uvea (the middle layer of the eye that consists of the iris, ciliary body and choroid). It can have many causes such as: eye injury, inflammatory diseases; and, exposure to toxic chemicals (pesticides and acids). The type of uveitis you have is classified by where inflammation occurs in the uvea:
- Anterior uveitis is inflammation of the iris (iritis) or the iris and ciliary body.
- Intermediate uveitis is inflammation of the ciliary body.
- Posterior uveitis is inflammation of the choroid.
- Diffuse uveitis (also called panuveitis) is inflammation of all areas of the uvea.
Symptoms of uveitis include:
- Eye redness
- Watery eyes
- Eye pain
- Light sensitivity
- Decreased vision
- Dark, floating spots in field of vision (floaters)
Uveitis can be acute or chronic, but patients should see their doctor as soon as possible as these diseases can lead to reduced vision or visual loss. Treatment is primarily aimed to try an eliminate inflammation, pain and prevent further tissue damage. Plans will vary depending on the type of uveitis and the causes.
Glaucoma
Glaucoma is the term used for a group of eye conditions resulting in optic nerve damage. These diseases cause abnormally high pressure inside the eye (intraocular pressure) and can cause vision loss.
Glaucoma is one of the leading causes of blindness worldwide. Glaucoma can damage vision so gradually patients may not notice any loss of vision until it is at an advanced stage. The primary type of glaucoma, primary open-angle glaucoma, does not have any noticeable signs or symptoms except gradual vision loss.
Early diagnosis and treatment is essential to minimize or prevent optic nerve damage. This will limit glaucoma-related vision loss.
It’s important for patient’s to get their eyes examined regularly.
Depending on the type of Glaucoma a patient is diagnosed with, there are many different causes of damage to the optic nerve. Generally, increased intra-ocular pressure is associated with the optic nerve damage. This is a characteristic of Glaucoma and loss of vision.
Primary open-angle Glaucoma
The drainage angle (formed by the cornea and the iris remains open) but the channels (trabecular meshwork) are partially blocked. This causes the reduced fluid drainage. This fluid then builds-up in the eye. Intra-ocular pressure gradually increases within the eye.
Damage to the optic nerve (caused by this process) does not cause symptoms or pain. It may happen so slowly that patient’s may lose a significant portion of their vision before they’re even aware of a problem.
Angle-closure Glaucoma
This occurs when the iris bulges forward. It causes narrowing or blockage of the drainage angle. This leads to inadequate fluid flow through the drainage angle. Large spikes in intra-ocular pressure can occur suddenly or gradually.
Individuals with an abnormally narrow drainage angle can be at risk of developing this form of Glaucoma.
The most common types of glaucoma have completely different symptoms.
Patients with primary open-angle glaucoma may notice the following symptoms:
- Gradual loss of peripheral vision, usually in both eyes
- Tunnel vision in the advanced stages
While patients with acute angle-closure glaucoma will notice the following symptoms:
- Eye pain
- Nausea and vomiting (accompanying the severe eye pain)
- Sudden onset of visual disturbance, often in low light
- Blurred vision
- Halos around lights
- Reddening of the eye
- Elevated intra-ocular pressure
- Aged 60 or over
- Family history of glaucoma – Having a family history of glaucoma means you have a greater risk.
- Medical conditions. Some conditions may increase your risk. (Diabetes, Heart diseases, Hypertension and Hypothyroidism).
- Co-existing eye conditions. Various eye conditions increase a patient’s risk. (Severe eye, Eye tumours, Retinal detachment, Eye inflammation and lens dislocation).
- Long-term corticosteroid use – Using corticosteroid medications (especially eye drops) chronically can increase your risk.
Tests that can be performed to diagnose Glaucoma include:
- Intraocular pressure checks – This is a simple, painless procedure that measures your internal eye pressure.
- Optic Nerve Examination – This is a check for damage in the optic nerve. Various uses instruments can be used and they look directly through the pupil to the back of the eye.
- Visual Field Test – This checks for visual field loss which has been caused by glaucoma. Specialised machines are used to test a patient’s visual field.
- Gonioscopy – Used to distinguish between open-angle glaucoma and angle-closure glaucoma. A special lens is placed on the eye to inspect the drainage angle.
The goal of treatment is to lower intraocular pressure. Depending on the condition, ophthalmologists will aim to lower eye pressure, improve drainage of fluid or lower the amount of fluid produced.
Glaucoma can’t be cured, and damage caused by the disease can’t be reversed.
Treatment and regular appointments can prevent visual loss. If vision loss has already occurred, treatment can slow or prevent further vision loss.
Eye Drops
Glaucoma treatment generally commences with medicated eye drops. It is important use the drops exactly as prescribed.
Oral medications
If eye drops alone don’t reduce the eye pressure to the desired level, the doctor may prescribe an oral medication.
Surgery
Surgery can be utilized to treat Glaucoma if the patient is in-tolerant to medications or if they’re ineffective. A single surgical procedure may not effectively lower the intra-ocular pressure eye pressure. Continuation of eye drops or combination of surgical intervention may be needed.
Surgeries that may be performed to treat glaucoma include:
Laser Trabeculoplasty
A procedure to treat open-angle glaucoma. The doctor uses a high-energy laser beam to open clogged drainage canals which helps fluid drain more easily from your eye.
Trabeculectomy
This procedure is performed in a day surgery or hospital. The retinal specialist will use small instruments to create an opening in the sclera. This allows the removal of a small piece of eye tissue so fluid can drain through the eye.
Drainage Implants
This surgery involves the insertion of a small tube in the eye to facilitate draining fluid to reduce the eye pressure.
Treating acute angle-closure glaucoma
Acute angle-closure glaucoma is a medical emergency. When diagnosed, urgent treatment is required to reduce the pressure. This will require both medication and laser surgery. A laser peripheral iridotomy is used to create a small hole in your iris. This allows the fluid to flow through the eye.
Macular Hole
Macular hole is a small break in the macula. This is located in the centre of the macula (which is the eye’s light-sensitive tissue), called the retina. This area provides the sharp, central vision needed for daily activities such as reading, driving, and fine detail vision like recognising a face.
There are different stages to this eye condition. They are:
- Foveal detachments (Stage I)
- Partial-thickness holes (Stage II)
- Full-thickness holes (Stage III)
The size of the hole and its location will determine how the patient’s vision is affected. Macular holes are caused when the vitreous slowly shrinks and pulls away from the retinal surface. This fluid contains many fine fibres that are attached to the surface of the retina. As a person gets older, the vitreous slowly shrinks causing it to pull away from the retina.
If the vitreous is strongly attached to the retina when pulling away, it can tear the retina. This creates the macular hole. Fluid then seeps through the hole onto the macula, causing symptoms of blurred and distorted central vision.
Depending on the severity on the condition, patients may experience:
- Slight distortion or blurring of central vision (during early stages).
- Straight lines and objects appearing wavy or bent.
- Difficulty with routine tasks such as reading or driving.
- Age – Primary risk factor and is more common in patients 60 or over.
- Short-sightedness (Myopia)
- History of retinal tears or detachments.
- Inflammation in the eye (such as Uveitis).
- Diabetes
If left untreated, a macular hole may lead to a detached retina. This is a medical emergency and Retinal Detachment require immediate specialist care to preserve the individual’s vision. Although some Macular holes can seal themselves, surgical intervention is usually required to improve vision.
Vitrectomy
A form of keyhole surgery where a small probe is used to remove the vitreous. Gas is injected into the eye to replace the fluid. This prevents it from pulling on the retina. This procedure is done as at day eye surgery using a local anaesthesia.
Pterygium
 A Pterygium (‘wing of tissue’) is an overgrowth of the conjuctiva that usually only covers the white of the eye onto the cornea. It usually presents in patients over the age of 45, although it has been known to occur during younger years. This is not a cancer as it is a discrete abnormality on the external surface of the eye.
A Pterygium (‘wing of tissue’) is an overgrowth of the conjuctiva that usually only covers the white of the eye onto the cornea. It usually presents in patients over the age of 45, although it has been known to occur during younger years. This is not a cancer as it is a discrete abnormality on the external surface of the eye.
Pterygium can grow at varying rates. They can grow rapidly, slowly, regress spontaneously and restart growing after a long period of time. Occasionally, it may encroach the pupil and enter the line of vision. Pterygium may grow on both eyes but they rarely grow more than once per eye.
Pterygia seem to be particularly common in Queensland. Queenslanders have one of the highest reported rates of occurrence in the world (up to 10%).
- Excessive sunlight exposure in the first 10 years of life.
- Living in a dry and/or dusty environment.
Most patients have no symptoms. Patients do sometimes experience:
- Dry Eyes
- Ocular Irritation
- Cosmetic changes, from the reddish lesion
Decrease in vision (Directly – If covering the line of sight. Indirectly – Changing the shape of the cornea.)
Significant numbers of patients complain of dry eyes and ocular irritation. This can actually predate the onset of the Pterygium. Others are just aware of the cosmetic disfigurement caused by the reddish wing like lesion growing onto the clear part of the front of the eye (the cornea).
Air conditioning, lack of sleep, sunlight, night shifts, and smoke can all aggravate a Pterygium increasing symptoms and redness.
It is important to note that a Pterygium can reduce vision indirectly by deforming the cornea (astigmatism) or directly by covering the direct line of sight through the pupil.
In most cases, no intervention is required. They generally don’t regress and patients should monitor any changes at home. If there are concerns about recent growth, this is a prompt for review by an eye care professional.
In those patients in whom redness is the main issue, the occasional use of an over the counter ‘eye whiteners’ can give temporary relief for important social occasions. Chronic use of these eye drops is not recommended as rebound redness on withdrawing these drops if used chronically.
The use of artificial tears (especially preservative free preparations) can achieve a similar if slower relief of irritation and redness and are often under used, even in eyes without dry eye symptoms.
Surgical excision of Pterygia is indicated for either cosmetic reasons or visual interference. In cases where surgery is undertaken to eradicate symptoms of irritation and dryness, these outcomes are less successful. This is because those symptoms generally predate Pterygium development and they can persist after removal.
The major complication is re-occurrence of the Pterygium. Simple excision re-occurrence rates have been reported as high as 40%. For excision with more advanced techniques, it is between 5 to 15%.
One such modern technique is to combine Pterygium removal with a conjunctival auto-graft along with wide dissection of tenons. The graft is secured with tissue glue from underneath the upper lid area which protects it from U.V sunlight. These all help improve clearance rate to ensure re-occurrence rates are as low as possible.

This pterygium extends to the pupil margin (a+b) however detailed mapping (c) shows a flattening effect of over 8 Dioptres encroaching the central visual axis and far past the pupil depicted as the dotted line. This impacts the vision particularly at night when the pupil is more dilated and more of the pterygium interferes with the enlarged central visual axis. Removal of the pterygium (d+e) removed the troublesome aberrations (f) in the vision and simplified his spectacle prescription.
Pterygium removal utilised a conjunctival graft prepared from non sun damaged conjunctiva under the upper lid. Using a conjunctival graft to cover the defect left after pterygium removal is the gold standard of care currently. The arrows (e) delineate the graft edge. This has been proven to reduce the pterygium recurrence rate from around 40-50% to less than 5%. This pterygium was secured using a tissue glue (d+e) rather than sutures which provides more comfort postoperatively. There is also some weak published evidence to suggest that the tissue glue may also reduce the chance of a recurrence even further compared to using sutures (2%).
Prevention is better than cure.
Things you can do to help reduce your risk of Pterygia include:
- Wearing sunglasses when possible. It is important they are labeled as compliant with Australian Standard (AS 1067.1 1990 Sunglasses and Fashion Spectacles). Also look for an EPF UV rating of either 9 or 10; these lenses transmit minimal UV radiation.
- Children should be kept out of the midday sun. For school children particularly of primary school age, sunglasses should be worn outdoors. Kids of all ages should wear broad-brimmed hats, strollers and baby buggies should have a sun visor and kids wear appropriate sunglasses from the earliest age coaxible.
Retinal Eye Conditions
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Retinal Tear or Detachment
Surgery is almost always used to repair a retinal tear, hole or detachment. Your ophthalmologist can tell you about the various risks and benefits of your treatment options. Together you can determine what treatment is best for you.
Retinal Vein Occlusion
Retinal Vein Occlusion (RVO) is a common vascular disorder of the retina.
Retinal vein occlusion is a blockage of the small veins that carry blood away from the retina. The retina is the layer of tissue at the back of the inner eye that converts light images to nerve signals and sends them to the brain.
Am I suitable?
Use our online tool to find out if you’re suitable for Laser Eye Surgery or cataract surgery.
