Cataract Surgery
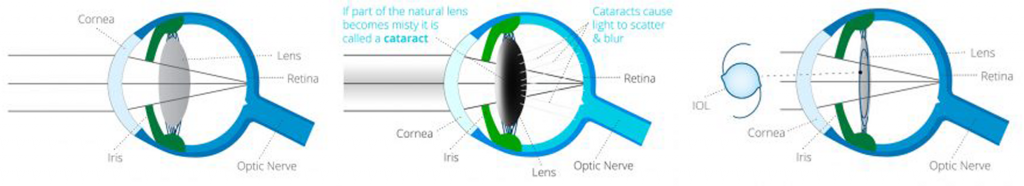
Cataract surgery, or refractive lens exchange surgery, is the procedure involving the removal of the cloudy lens along and the insertion of an artificial intraocular lens to take its place. There are several different types of procedures to remove the cataract.
Cataract Surgery
This procedure involves the removal of the cloudy lens along with the insertion of an artificial intraocular lens to take its place. There are several different types of procedures to remove the cataract.
Phacoemulsification is the standard procedure where the cloud lens is removed through a small incision (@2mm) in the cornea. A circular window is formed in the thin clear membrane (capsule) holding the cataract. A thin probe is inserted into the eye which emulsifies the lens matter. These tiny fragments are then aspirated from the eye. Once the cataract is removed, an artificial lens implant is placed in the same capsular bag that the cataract previously occupied. This intraocular lens is essential to help your eye focus after surgery.
It is unusual to require a stitch in the eye at the end of the operation because the incision is so small it is nearly always self-sealing. Eyes that have a thin corneal wall (keratoconus) tend to be floppy and these do require a stitch to avoid wound sag and degradation of the expected visual outcome.
This procedure requires the use of anaesthetic around the eye and sedation and is often referred to as “Twilight Sedation”. It tends to induce amnesia before and after surgery however, if you want to remember something, it is likely that you will. This amnesia is the reason why we insist that you have a carer overnight before admitting you for surgery. For a clear demonstration, please view the following link: Why You Need a Carer Overnight.
Depending on an individual’s needs, there are several different intraocular lens options available to suit a variety of demands. The information below is a synopsis of options available to a patient. Consultation with a specialist Cataract & Refractive Surgeon is always required to ensure the patient is suitable for a specific lens type.
This utilises a lens with a single focal point, usually set for distance in each eye. It gives good binocular vision over a useful range. If a patient is happy to wear intermediate and reading glasses, then this is the most common option and is usually the only option offered in the public health system.
Two different standard lenses (one eye set for distance vision, the other set for intermediate distance vision), then this is a suitable option for those patients who may have had prior experience of it in spectacles or contact lenses. It breaks down stereopsis (3D perception) and you will still need reading glasses for fine print. In my practice I reserve this for those who have had experience of this naturally or in contact lenses, for most others tolerance is untested and cataract surgery is not the best place to first try it. If one were to insist, perhaps a previous psychiatric will be required.
One eye is set for distance and the other for an intermediate focus point. This is well tolerated as it still provides some stereopsis (3D perception) and useful range of vision but you will still need reading glasses for all near tasks and occasionally for visual tasks performed at an intermediate distance. This is another very common choice and if the patient is happy to wear reading glasses, you have a very happy patient indeed.
These lenses move when implanted in the eye and try to mimic the body’s own natural lens movements. They aim to give good vision over a range of distances. In reality, because they move their resting point in the eye is more unpredictable and more people end up a little more short or long sighted than they bargained for. Additionally, most do not move enough and so you still need reading glasses for near. They also tend to move too slowly so there is a significant lag time ( speed of accommodation ) when you look from the distance to focus on something up close which can be quite frustrating. Others accommodating lenses move too easily in a bid to obtain more near vision and there are a few anecdotes that with a good sneeze one can apparently be left short sighted unexpectedly on the freeway!
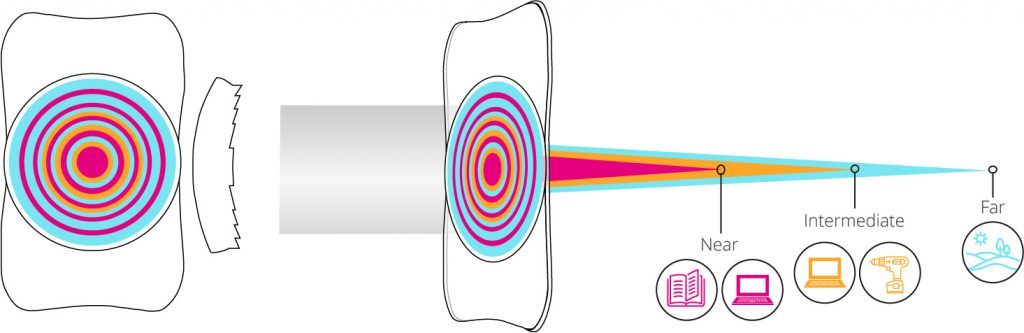
This lens type has both a distance component and reading component. This works in a similar manner to bi-focal prescription glasses except that in glasses the patient looks from the distance into the near segment and thus the whole vision sees only one in focus image at a time. With multifocal lens implants both the distance and the near vision are in focus at the same time in the eye. When one looks in the distance there is usually nothing obstructing the view at near. When looking at a book for near vision, the book blocks the distance image. Multifocal implants offer patients relative spectacle independence. The same operation is offered as a lifestyle choice to patients without cataract who simply want the greater freedom from wearing glasses. A period of adaptation is required and the compromise with this lens is often noted at night with ghosting, halos and excess of stray scattered light in the vision. This is most notable when viewing a point source of light at night (e.g. a car headlight).
Not all multifocal implants are the same. Some versions are based on simple prism technology with concentric rings of distance and near which have been around for 25 years. These diffractive (or extended depth of focus) multifocal implants produce marked halos and light scatter particularly troublesome when night driving. The adaptation phase is typically 6-12 months and a significant percentage of individuals remain dissatisfied and less confident with night driving one year after surgery. There is also an associated significant explant rate when advocated to the wrong type of patient. This technology has improved but not eliminated these compromises. It has a place, particularly for those who have distance, intermediate and near tasks to perform.
Personally I tend to advocate segmental multifocal implants. The adaptation phase is 4-8 weeks typically and the impact on night driving confidence is consistently reported as much less. Here the near vision is inferior to the distance segment when placed in the eye. The aberrations in the vision happen in the vertical meridian (inferiorly) as opposed to the diffractive multifocal implants that produce the 360 degree multiple ring halo effects.

Patients with high levels of astigmatism can utilise Toric Lens technology, which is designed to neutralise any astigmatism arising from the cornea. Toric lenses correct distortions in one particular meridian/ axis. They can be found in single distance vision lenses and in multifocal implants. Correcting astigmatism is the second most important optical correction impacting the quality of the unaided visual outcome after correcting defocus (how long or short sighted a patient is).
Refractive Cataract Surgery PLUS
Contact the practice for details on Refractive Cataract Surgery PLUS
Refractive Lens Exchange Surgery
This procedure involves the removal of the cloudy lens along with the insertion of an artificial intraocular lens to take its place. There are several different types of procedures to remove the cataract.
Phacoemulsification is the standard procedure where the cloud lens is removed through a small incision (@2mm) in the cornea. A circular window is formed in the thin clear membrane (capsule) holding the cataract. A thin probe is inserted into the eye which emulsifies the lens matter. These tiny fragments are then aspirated from the eye. Once the cataract is removed, an artificial lens implant is placed in the same capsular bag that the cataract previously occupied. This intraocular lens is essential to help your eye focus after surgery.
It is unusual to require a stitch in the eye at the end of the operation because the incision is so small it is nearly always self-sealing. Eyes that have a thin corneal wall (keratoconus) tend to be floppy and these do require a stitch to avoid wound sag and degradation of the expected visual outcome.
This procedure requires the use of anaesthetic around the eye and sedation and is often referred to as “Twilight Sedation”. It tends to induce amnesia before and after surgery however, if you want to remember something, it is likely that you will. This amnesia is the reason why we insist that you have a carer overnight before admitting you for surgery. For a clear demonstration, please view the following link: Why You Need a Carer Overnight.
Depending on an individual’s needs, there are several different intra-ocular lens options available to suit a various demands. The information below is a synopsis of options available to a patient. Consultation with a specialist Cataract & Refractive Surgeon is always required to ensure the patient is suitable for a specific lens type.
This utilises a lens with a single focal point, usually set for distance in each eye. It gives good binocular vision over a useful range. If a patient is happy to wear intermediate and reading glasses, then this is the most common option and is usually the only option offered in the public health system.
Two different standard lenses (one eye set for distance vision, the other set for intermediate distance vision), then this is a suitable option for those patients who may have had prior experience of it in spectacles or contact lenses. It breaks down stereopsis (3D perception) and you will still need reading glasses for fine print. In my practice I reserve this for those who have had experience of this naturally or in contact lenses, for most others tolerance is untested and cataract surgery is not the best place to first try it. If one were to insist, perhaps a previous psychiatric will be required.
One eye is set for distance the other for an intermediate focus point. This is well tolerated as still provides some stereopsis (3D perception) and useful range of vision but you will still need reading glasses for all near tasks and occasionally for visual tasks performed at an intermediate distance. This is another very common choice and if the patient is happy to wear reading glasses, you have very happy patient indeed.
These are lenses move when implanted in the eye and try to mimic the body’s own natural lens movements. They aim to give good vision over a range of distances. In reality, because they move their resting point in the eye is more unpredictable and more people end up a little more short or long sighted than they bargained for. Additionally, most do not move enough and so you still need reading glasses for near. They also tend to move too slowly so there is a significant lag time ( speed of accommodation ) when you look from the distance to focus on something up close which can be quite frustrating. Others accommodating lenses move too easily in a bid to obtain more near vision and there are a few anecdotes that with a good sneeze one can apparently be left short sighted unexpectedly on the freeway!


Patients with high levels of astigmatism can utilise Toric Lens technology, which is designed to neutralise any astigmatism arising from the cornea. Toric lenses correct distortions in one particular meridian/ axis. They can be found in single distance vision lenses and in multifocal implants. Correcting astigmatism is the second most important optical correction impacting the quality of the unaided visual outcome after correcting defocus (how long or short sighted a patient is).
Standard Cataract Surgery
This procedure involves the removal of the cloudy lens along with the insertion of an artificial intraocular lens to take its place. There are several different types of procedures to remove the cataract.
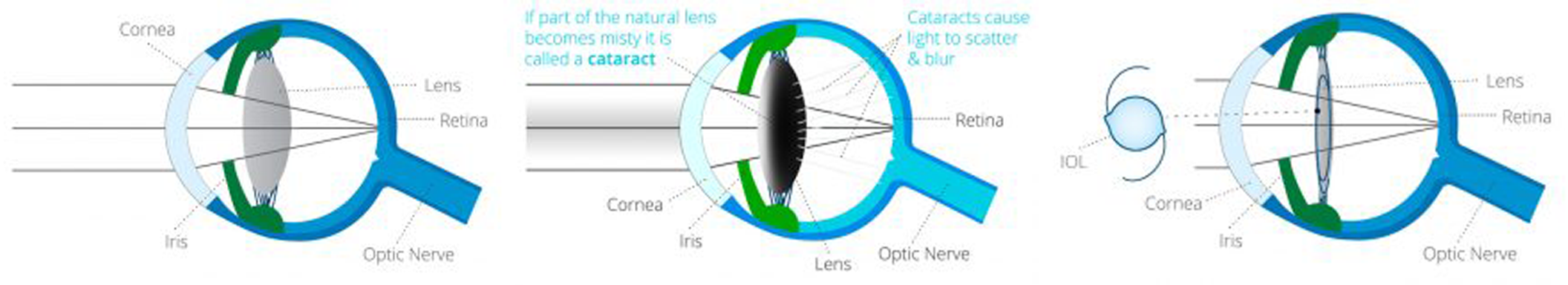
Phacoemulsification is the standard procedure where the cloud lens is removed through a small incision (@2mm) in the cornea. A circular window is formed in the thin clear membrane (capsule) holding the cataract. A thin probe is inserted into the eye which emulsifies the lens matter. These tiny fragments are then aspirated from the eye. Once the cataract is removed, an artificial lens implant is placed in the same capsular bag that the cataract previously occupied. This intraocular lens is essential to help your eye focus after surgery.
It is unusual to require a stitch in the eye at the end of the operation because the incision is so small it is nearly always self-sealing. Eyes that have a thin corneal wall (keratoconus) tend to be floppy and these do require a stitch to avoid wound sag and degradation of the expected visual outcome.
This procedure requires the use of anaesthetic around the eye and sedation and is often referred to as “Twilight Sedation”. It tends to induce amnesia before and after surgery however, if you want to remember something, it is likely that you will. This amnesia is the reason why we insist that you have a carer overnight before admitting you for surgery. For a clear demonstration, please view the following link: Why You Need a Carer Overnight.
Depending on an individual’s needs, there are several different intra-ocular lens options available to suit a various demands. The information below is a synopsis of options available to a patient. Consultation with a specialist Cataract & Refractive Surgeon is always required to ensure the patient is suitable for a specific lens type.
This utilises a lens with a single focal point, usually set for distance in each eye. It gives good binocular vision over a useful range. If a patient is happy to wear intermediate and reading glasses, then this is the most common option and is usually the only option offered in the public health system.
Two different standard lenses (one eye set for distance vision, the other set for intermediate distance vision), then this is a suitable option for those patients who may have had prior experience of it in spectacles or contact lenses. It breaks down stereopsis (3D perception) and you will still need reading glasses for fine print. In my practice I reserve this for those who have had experience of this naturally or in contact lenses, for most others tolerance is untested and cataract surgery is not the best place to first try it. If one were to insist, perhaps a previous psychiatric will be required.
One eye is set for distance the other for an intermediate focus point. This is well tolerated as still provides some stereopsis (3D perception) and useful range of vision but you will still need reading glasses for all near tasks and occasionally for visual tasks performed at an intermediate distance. This is another very common choice and if the patient is happy to wear reading glasses, you have very happy patient indeed.
These are lenses move when implanted in the eye and try to mimic the body’s own natural lens movements. They aim to give good vision over a range of distances. In reality, because they move their resting point in the eye is more unpredictable and more people end up a little more short or long sighted than they bargained for. Additionally, most do not move enough and so you still need reading glasses for near. They also tend to move too slowly so there is a significant lag time ( speed of accommodation ) when you look from the distance to focus on something up close which can be quite frustrating. Others accommodating lenses move too easily in a bid to obtain more near vision and there are a few anecdotes that with a good sneeze one can apparently be left short sighted unexpectedly on the freeway!
Patients with high levels of astigmatism can utilise Toric Lens technology, which is designed to neutralise any astigmatism arising from the cornea. Toric lenses correct distortions in one particular meridian/ axis. They can be found in single distance vision lenses and in multifocal implants. Correcting astigmatism is the second most important optical correction impacting the quality of the unaided visual outcome after correcting defocus (how long or short sighted a patient is).
Standard Cataract Surgery Plus
This procedure involves the removal of the cloudy lens along with the insertion of an artificial intraocular lens to take its place. There are several different types of procedures to remove the cataract.
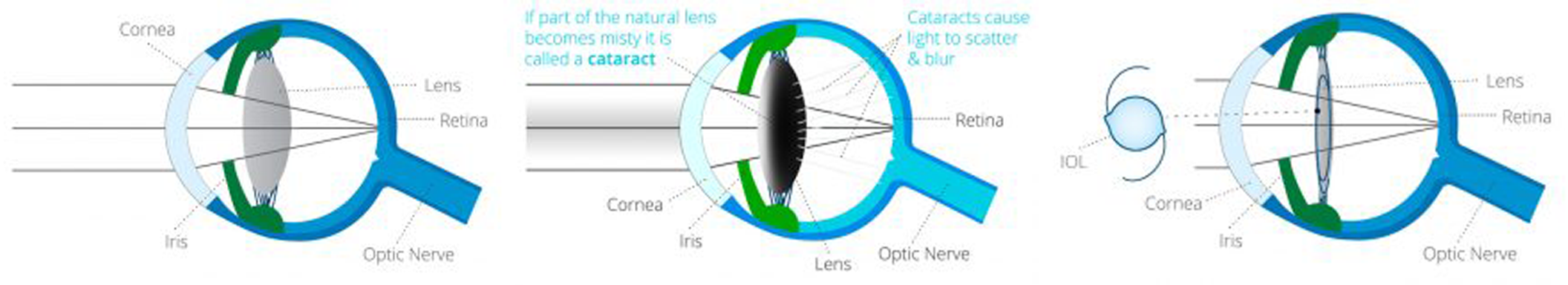
Phacoemulsification is the standard procedure where the cloud lens is removed through a small incision (@2mm) in the cornea. A circular window is formed in the thin clear membrane (capsule) holding the cataract. A thin probe is inserted into the eye which emulsifies the lens matter. These tiny fragments are then aspirated from the eye. Once the cataract is removed, an artificial lens implant is placed in the same capsular bag that the cataract previously occupied. This intraocular lens is essential to help your eye focus after surgery.
Advanced aging changes have an increased risk of converting from dry to wet after routine cataract surgery and can be an excess of associated vision loss. The non-standard use of anti-VEGF agents (agents that reduce the chance of abnormal blood vessels developing and bursting) may be helpful in reducing the excess risk of vision loss during cataract surgery. Ask your Eye Surgeon if this is relevant to you.
Diabetic retinopathy needs to be controlled before and after cataract surgery. In adequate control can lead to sight threatening vision changes due to abnormal new vessels growing on the retina and the development of a boggy, swollen macular. Ask you Eye Surgeon if this is relevant to you.
Patients with Fuch’s are at excess risk of corneal clouding and visual loss after cataract surgery. As well as overt corneal clouding and reduced vision, it is also responsible for a mediocre visual outcome, after routine cataract surgery. New cataract surgical techniques and new corneal transplantation techniques have improved the outlook for this patient group. Ask your Surgeon if this is relevant to you at the time of planning your cataract surgery.
There is increasing evidence for the use of glaucoma stents inserted during cataract surgery, patients with poor glaucoma control on two or more drops should ask their Eye Surgeon if this is relevant to them at the time of planning your cataract surgery.
It is unusual to require a stitch in the eye at the end of the operation because the incision is so small it is nearly always self-sealing. Eyes that have a thin corneal wall (keratoconus) tend to be floppy and these do require a stitch to avoid wound sag and degradation of the expected visual outcome.
This procedure requires the use of anaesthetic around the eye and sedation and is often referred to as “Twilight Sedation”. It tends to induce amnesia before and after surgery however, if you want to remember something, it is likely that you will. This amnesia is the reason why we insist that you have a carer overnight before admitting you for surgery. For a clear demonstration, please view the following link: Why You Need a Carer Overnight
Targeting an eye with keratoconus to see well unaided after routine cataract surgery is more difficult than in a normal eye. Most routinely used formulae to calculate the correct lens power for an eye make assumptions and the more severe the keratoconus the more these assumptions no longer hold. Ask your Surgeon if this is relevant to you at the time of planning your cataract surgery.
Patients with a lazy eye can have a variable improvement at the time of catract surgery. Your Eye Surgeon should make every attempt to discern your dominant from your non-dominant eye. The lazy eye patient often finds it difficult to functionally adapt if the lazy eye ends up seeing better in the distance than the dominant eye. Ask your Surgeon if this is relevant to you at the time of planning your cataract surgery.
These are lenses move when implanted in the eye and try to mimic the body’s own natural lens movements. They aim to give good vision over a range of distances. In reality, because they move their resting point in the eye is more unpredictable and more people end up a little more short or long sighted than they bargained for. Additionally, most do not move enough and so you still need reading glasses for near. They also tend to move too slowly so there is a significant lag time ( speed of accommodation ) when you look from the distance to focus on something up close which can be quite frustrating. Others accommodating lenses move too easily in a bid to obtain more near vision and there are a few anecdotes that with a good sneeze one can apparently be left short sighted unexpectedly on the freeway!
Patients with high levels of astigmatism can utilise Toric Lens technology, which is designed to neutralise any astigmatism arising from the cornea. Toric lenses correct distortions in one particular meridian/ axis. They can be found in single distance vision lenses and in multifocal implants. Correcting astigmatism is the second most important optical correction impacting the quality of the unaided visual outcome after correcting defocus (how long or short sighted a patient is).
Am I suitable?
Use our online tool to find out if you’re suitable for Laser Eye Surgery or cataract surgery.
